Gut dysbiosis and cows’ milk protein allergy (CMPA) — is there a link?

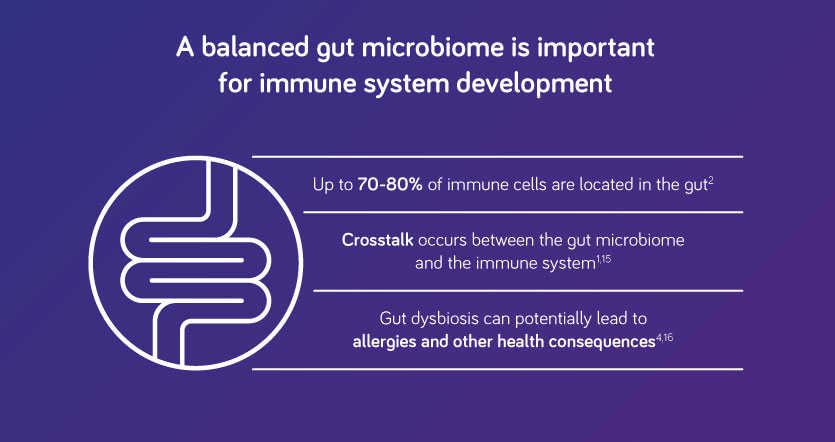
Gut dysbiosis occurs when there is an imbalance of bacteria in the gut microbiota, the community of bacteria that inhabit the gut.1 With 70-80% of immune cells residing in the gut,2 the gut microbiota plays an essential role in health. Gut microbiota dysbiosis in infants has the potential to increase the risk of food allergies such as cows’ milk protein allergy (CMPA).1
There is a growing body of evidence on the role of prebiotics and probiotics in allergy management. Can a unique synbiotic – a combination of prebiotics and probiotics – help to rebalance the gut microbiota and support the immune system?
What is gut microbiota dysbiosis? Gut dysbiosis is often defined as an imbalance of the gut microbiota.1 The gut microbiome provides many useful functions including protection from harmful pathogens, strengthening the body’s immune defences, and performing vital metabolic tasks.3 When the composition of the gut microbiota is disturbed, these vital functions can be impaired, potentially leading to disease.1 Gut dysbiosis can be due to a loss of beneficial bacteria, an increase in pathogenic microbes or a loss of overall diversity.1
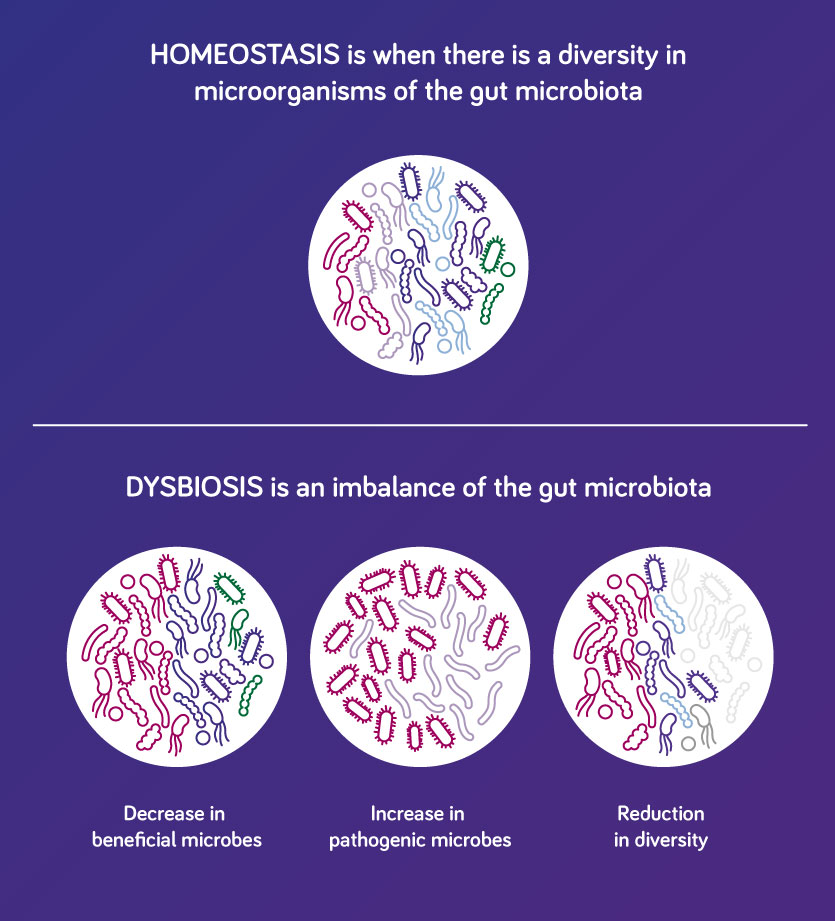
Adapted from Peterson and Round, 2014.1
What causes gut microbiota dysbiosis in infants? Early life is a critical time for the development of the gut microbiome and hence the infant gut is particularly vulnerable to dysbiosis. There are several factors, which influence the composition of the gut microbiome in infants including:1,4-6
- Gestational age
- Maternal environment
- Delivery mode (vaginal or caesarean)
- Nutrition (breast or formula feeding)
- Use of antibiotics
- Diet
- Air pollution
- Genetics
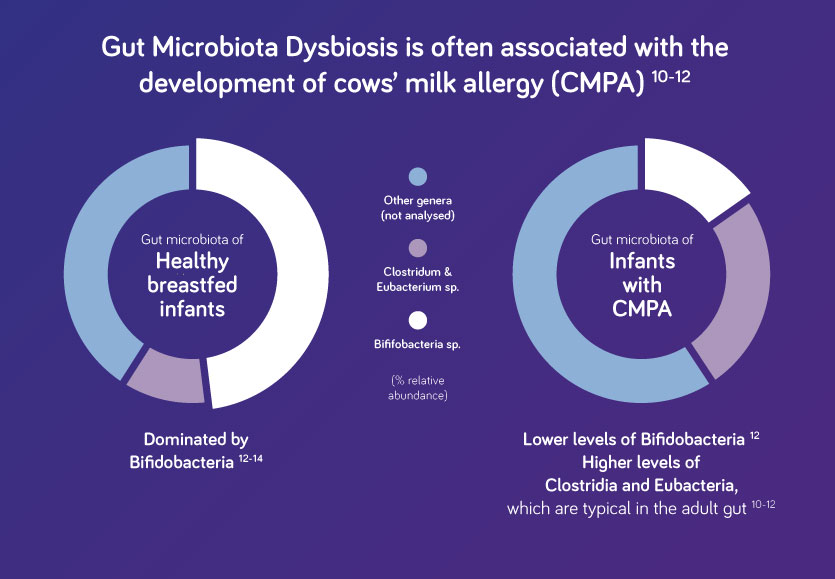
Genetic factors and changes in environmental factors can alter the composition of the gut microbiome, leading to dysbiosis.1 What is the link between gut microbiota dysbiosis and allergy? Gut microbiota dysbiosis has been reported in infants with allergic conditions such as cows’ milk protein allergy (CMPA). In healthy, breast-fed infants, the gut is typically dominated by a group of beneficial bacteria known as bifidobacteria. These bacteria are first transmitted from the mother during birth and via breast milk.7–9 In infants with allergic conditions, environmental factors can affect the composition of the gut microbiota. Infants with CMPA often have lower levels of bifidobacteria in their gut microbiota compared with healthy, breast-fed infants.9 It is currently thought that gut dysbiosis can potentially lead to development of allergies and other health consequences in later life.1
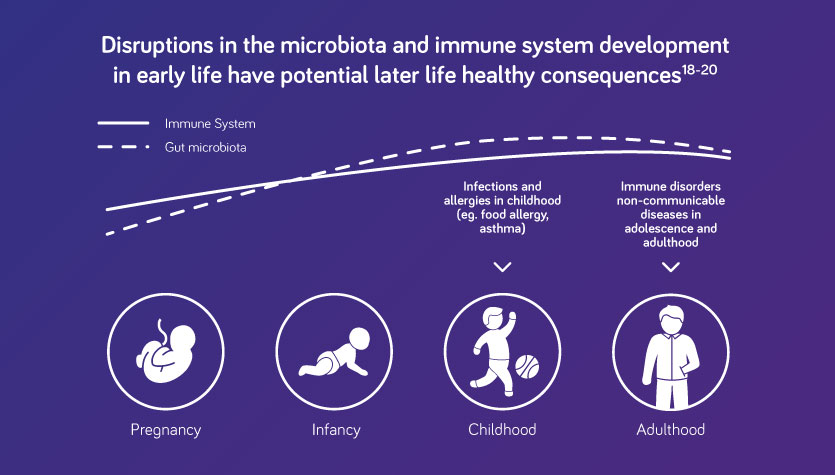
Can gut microbiota dysbiosis affect the development of the immune system? Early life is a critical time for both the development of the immune system and the gut microbiota. The immune system develops quickly during the first 1000 days of life and it is well known that crosstalk occurs between the immune system and gut microbiota. Gut microbiota dysbiosis therefore has the potential to affect development of the immune system, with the potential to lead to allergies, such as CMPA, and other health consequences such as asthma, metabolic syndrome, cardiovascular disease and obesity.4,15–17
Can gut microbiota dysbiosis lead to allergic disease such as cows’ milk protein allergy in infants? Gut microbiota dysbiosis is thought to play a role in the development of food allergies such as cows’ milk protein allergy (CMPA) in early life. Several studies have shown that gut dysbiosis in infants may delay the development of oral tolerance, a process in which the immune response to food protein is suppressed. Disruption of oral tolerance has the potential to lead to the development of food allergies.16 Gut dysbiosis in early life has also been linked to the development of several diseases including asthma, metabolic syndrome, cardiovascular disease and obesity.17
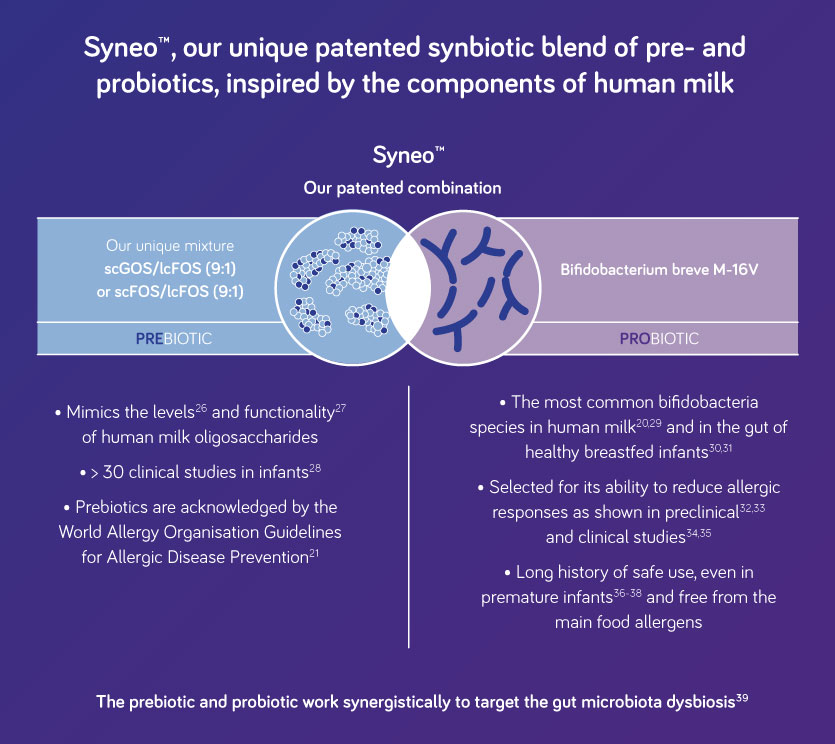
Can we shift the balance back to a healthy gut microbiota? Human milk contains both naturally occurring prebiotics such as human milk oligosaccharides (HMOs) as well as beneficial bacteria (probiotics). Both these elements help promote a healthy gut microbiota and support immune system development.16,17 If breastfeeding is not possible, the addition of a unique prebiotic combination and a probiotic – known as synbiotics – to infant formula, has been shown to rebalance the gut microbiome and promote oral tolerance, potentially reducing the risk of allergic disease.20,23,24
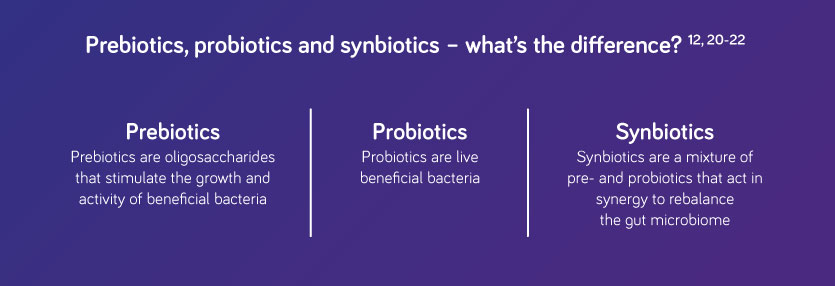
Why consider a unique synbiotic blend for cows’ milk protein allergy? A growing body of clinical evidence suggests that a unique synbiotic blend can have a beneficial effect in infants at risk of, or living with, food allergy such as CMPA.12,23,24 In recognition of the potential benefits of pre- and probiotics the World Allergy Organisation Guideline Panel suggests that pre and probiotic supplementation be considered for infants at risk of allergy if they are not exclusively breastfed.21,22 Presently, most probiotic-containing infant formula comprise Bifidobacterium species and/or lactic acid bacteria such as Lactobacillus species,25 which are generally regarded as safe and permitted in food for use under the Food Standards Australia and New Zealand Regulations. In the last decade, different prebiotic mixtures of galacto-oligosaccharides (GOS) and fructo-oligosaccharides (FOS) have been studied for their beneficial effects in infants at risk of, or living with, food allergy. Clinical research on prebiotic infant formula consisting of short-chain (sc) GOS and long-chain (lc) FOS, scGOS/lcFOS in a ratio of 9:1 — resembling the oligosaccharide components of human milk in both in quantity and diversity— showed benefits linked to modulation of the gut microbiota and the immune system, reduced incidence of infections, and stool softening.25 Selected Nutricia products for the treatment of cows’ milk protein allergy contain a unique patented synbiotic blend of prebiotics (encompassing the scGOS/lcFOS (9:1)) and probiotics (Bifidobacterium breve M16V)—inspired by the components of human milk.
Nutricia Global Conference
Featuring 60 international experts, the conference covered a range of topics including education and insight into innovative approaches to understanding and managing CMPA in infants. Sign up to receive content from the Nutricia Global Conference.
Learn morePetersen C and Round L. Cellular Microbiology 2014;16(7):1024–33.Vighi G et al. Clin Exp Immunol. 2008;153 Suppl 1(Suppl 1):3–6.O’Hara AM, Shanahan F. EMBO Rep. 2006 Jul;7(7):688–93.Prescott SL. J Allergy Clin Immunol. 2013;131(1):23–30.Kim BJ et al. Allergy Asthma Immunol Res. 2014;6(5):389–400.Azad MB et al. BJOG. 2016;123(6):983–93.Jeurink PV et al. Benef Microbes. 2013;4(1):17–30.Bäckhed F et al. Cell Host Microbe. 2015;17(5):690-703.Kirjavainen P et al. Gut 2002;51:51–5.Berni Canani R et al. ISME J 2016;3:742–50.Thompson-Chagoyan OC et al. Pediatr Allergy Immunol 2010;21:e394–400.Candy DCA et al. Pediatr Res. 2018;83(3):677–86.Harmsen HJ, et al. J Pediatr Gastroenterol Nutr. 2000;30(1):61–67.Scholtens PAMJ, et al. J. Annu Rev Food Sci Technol. 2012;3(1):425–447.McDermott AJ, Huffnagle G. Immunology 2013;142:24–31.Azad MB et al. Clin Exp Allergy. 2015;45(3):632–43.Carding S et al. Microb Ecol Health Dis. 2015;26:26191.West CE et al. J Allergy Clin Immunol. 2015;135(1):3–13.Walker WA et al. Pediatr Res. 2015;77(1–2):220–8.Martin R et al. Benef Microbes. 2010;1(4)367–82.Cuello-Garcia CA et al. World Allergy Organ J. 2016;9:10.Fiocchi A et al. World Allergy Organ J. 2015;8:4.Fox AT et al. Clin Transl Allergy. 2019;9:5.Van der Aa LB et al. Clin Exp Allergy. 2010;40:795–804.Salminen et al. Nutrients. 2020;12(7):1952.Kunz C et al. Annu Rev Nutr. 2000;20(1)699–722.Oozeer R et al. Am J Clin Nutr. 2013;98(2):561S–71S.Nutricia, Data on file.Soto A et al. J Pediatr Gastroenterol Nutr. 2014;59(1):78–88.Matsuki T et al. Appl Environ Microbiol. 1999;65(10):4506–12.Mikami K et al Pharmaceuticals. 2012;5(6):629–42.Inoue Y et al. Biol Pharm Bull. 2009;32(4):760–3.Hougee S et al. Int Arch Allergy Immunol. 2010;151(2):107–17.Hattori K et al. Arerugi. 2003;52(1):20–30.Taniuchi S et al. J Appl Res. 2005;5(2):387–96.Akiyama K et al. Acta Neonatol Jpn. 1994;30:257–63.Yamada T et al. Acta Neonatol Jpn. 2002;38:294.Patole SK et al. PloS One. 2016;11(3):e0150775.Schouten B et al. J Nutr. 2009;139:1398–403.
Support for you and your patients
Join now and learn about our education events, research initiatives and evidence-based resources – furthering your professional development and clinical practice.
Support for you and your patients
Support for you and your patients
Join now and learn about our education events, research initiatives and evidence-based resources – furthering your professional development and clinical practice.